As a biomedical engineer, Brian Diekman is committed to figuring out exactly why and how the tissue between our joints degrades over time. His research may lead to less pain and more mobility for millions of Americans living with osteoarthritis.
When Brian Diekman talks to friends and family about his research at UNC-Chapel Hill, he often hears the same question again and again: will this happen to me?
“Osteoarthritis is such a prevalent disease,” Diekman says. “I am always struck by the number of people who worry about developing it or are already living with it.”
Over 30 million Americans suffer from osteoarthritis (OA), or the degeneration of joint cartilage. Since there is no cure, the disease must be managed with a mixture of therapies and medications. But many people living with osteoarthritis are living in pain, according to Diekman. “The drugs are just not there yet,” he says. “We don’t have good drugs because we don’t fully understand how OA develops. A lot of different factors contribute to OA, and it’s difficult to pull them apart.”
Diekman wants to change that. Using novel approaches, his lab examines the basic biology of aging, as well as joint injuries, and how those complex processes contribute to osteoarthritis.
Beyond wear and tear
“When we talk about OA, you hear a lot of people using the term ‘wear and tear,’” Diekman says. “But that’s really an oversimplification of what’s going on — our joints don’t just ‘wear out.’ There are a number of biological factors at play.”
While it’s easy to think of cartilage as a spongy shock absorber, Diekman says it is more accurate to picture it as a high-quality matrix of tissues. “Cartilage has many exquisite properties that make it capable of withstanding enormous loads.”
As our bodies age, inflammation becomes more common throughout the body, including the cells in our joints. One source of these inflammatory factors is cells that have become senescent and no longer divide.
“We sometimes think of senescent cells as zombie cells,” Diekman says. “They are still hanging around, but they’re causing more harm than good. They can cause the surrounding cartilage tissue to degrade.”
Diekman and his colleagues are working hard to better understand how senescence emerges in the joint. By figuring out exactly which cells will become senescent, Diekman and his team can provide the scientific basis for creating more effective drugs.
“We want to kill the senescent cells while leaving the other cells intact.”
To achieve this goal, Diekman has established a unique collaboration.
The right tools
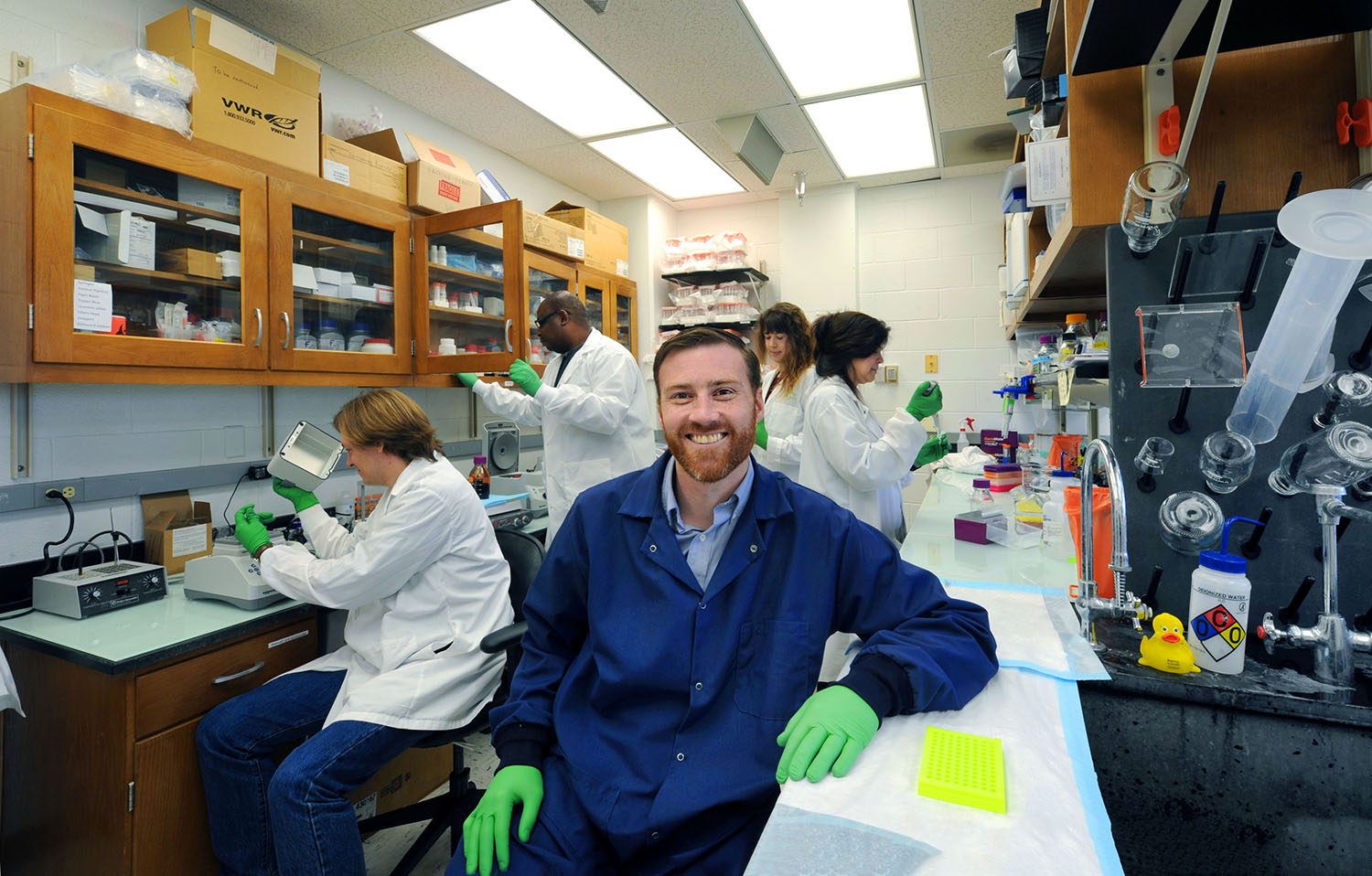
Diekman holds a dual appointment in the Thurston Arthritis Research Center (TARC) in the UNC School of Medicine and the department of biomedical engineering (BME) in UNC’s College of Arts & Sciences. BME is a joint-department between UNC and NC State. He describes his position as the perfect marriage of his areas of expertise.
“At TARC, we have experts studying every component of the disease. And then in BME we build tools to help prevent or mitigate components of the disease,” he says. “The ability to access both of those worlds and bring them together is ideal.”
Some biomedical engineers working in this field build tissues to insert directly into the degraded joints of patients with severe cases of OA.
“We use a lot of the same techniques, like stem cells and genome editing,” Diekman says. “But we have a different take on it.” Instead of making tissues to put into a patient’s joint, they make tissues to better understand how the disease functions.
The ability to examine the degeneration of a human joint within the confines of a petri dish is an innovation only available at a university like Carolina, according to Diekman.
“UNC has a particular concentration of researchers in the scientific areas that support our lab’s goals,” he says.
Working with other regenerative medicine experts in BME enables Diekman to execute precise and efficient research experiments. He is particularly grateful for the Polacheck Lab at UNC which specializes in building microfluidic devices to recreate the physical environment of the body in a petri dish.
“Because UNC has a strong culture of collaboration among faculty and learners of all career stages, I am able to actually harness all of the knowledge I am surrounded by to improve the quality of our research.”
Delivering better solutions
Helping people has always been at the core of Diekman’s desire to pursue science. He credits his parents for serving as excellent role models.
“My father was a professor of animal science, and my mother worked in social justice and community development,” he says. “So, I saw the benefits of academic research and how it can be personally fulfilling, but also how important it is to work toward something that can make a direct impact on people.”
Diekman’s father-in-law is a perfect example.
“He has been following my research more closely than most,” Diekman says. “For years, every time we got together, he asked, ‘do you have something for me, or am I going to have to get my hip replaced?’”
While his father-in-law has now had both hips replaced, Diekman hopes treatments for osteoarthritis in the future will not require total joint replacements.
“People are asking for better solutions,” he says. “We want to deliver them.”
By Mary Lide Parker, College of Arts & Sciences
